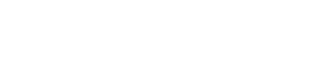
BUFFALO, N.Y. — Congressman Brian Higgins is making his objections known about a decision some Western New York insurance companies have made to stop covering the cost of some COVID-19 testing.
Three big insurers in Western New York have said they will not cover the cost of non-medically necessary tests, such as the ones that are required for some employment or return to the classroom.
On its website, Univera Healthcare wrote: "Testing that is ordered or performed solely for purposes of pandemic control or re-opening the economy, and not based on a determination by an attending provider that the test is medically appropriate for the diagnosis and treatment of an individual member, is not covered."
Dr. Thomas Schenk, Blue Cross Blue Shield 's Chief Medical Officer said "Back to work tests are an employer's option," and, "It's extremely important for community members to understand that if their employer requires them to get a COVID test before they can return to work or school, they should take advantage of New York State or county-coordinated testing sites."
In a press release, Congressman Higgins administration said COVID tests were previously covered for anyone who needed them, with or without symptoms.
However, the CARES act was amended in June by the Trump Administration to no longer require insurance providers to cover non-medically necessary tests.
Higgins wrote letters to both the Department of Labor, Treasury and Health and Human Services and Western New York insurers addressing his concerns.
"The lack of a national testing plan from this administration has meant that states and localities have been largely left to develop testing protocols on their own and scramble for what testing supplies they can get in the absence of national leadership. It is unconscionable for your departments to now also allow private insurance companies to abdicate their fair share of responsibility to their members and our communities by explicitly declaring that coverage of COVID-19 testing is not required under certain circumstances," Higgins said in his letter to the Department of Labor, Treasury and Health and Human Services.
Frank Sava, Director of Corporate Communications for Independent Health, released a statement that said in part, "Based on federal guidance, health plans are not required to cover COVID-19 testing when it is to screen for "return to work/school" purposes or for public health surveillance."
Representatives from each insurance company noted that they will continue to cover medical diagnostic testing for COVID-19.
You can access free COVID-19 diagnostic and antibody testing, even if you are asymptomatic through the Erie County Department of Health.
Full Insurance Provider Statements:
Blue Cross Blue Shield of WNY:
"Recent reports about health insurers not covering employer-required, back-to-work COVID-19 testing for healthy workers are incomplete, and therefore misleading.
There has been no change in our policy regarding occupational testing and public-health screening, and the policy follows what the vast majority of health insurers nationally are doing as well. The tests that are in question are ones that are mandatory for employment or to return to the classroom.
At BlueCross BlueShield of Western New York, we have and will continue to cover all medically necessary testing and treatment for our members. That has been the case since the pandemic exploded here in March. We still cover all testing recommended by a doctor, or other health care provider, because of direct exposure, travel exposure, or symptoms.
Back-to-work tests are an employer’s option. Many other employers will simply ask their colleagues to fill out the now-familiar symptoms-disclaimer form, and/or take their temperature upon entering the workplace.
It’s extremely important for community members to understand that if their employer requires them to get a COVID test before they can return to work or school, they should take advantage of New York State or county-coordinated testing sites throughout Western New York. Many of these sites presently allow for free, same-day appointments with a quick turnaround on results. Also important, when individuals are symptom-free and testing is optional, it’s safer for them to utilize drive-thru sites to limit their exposure to any other viruses and maintain their health.
BlueCross BlueShield is not standing on the sidelines in this fight. We have covered and will continue to cover the full cost of COVID-19 treatment, regardless of where care is provided in the United States; we eliminated prior authorization requirements for medically necessary COVID-19 testing and treatment; we cover the full cost for all telehealth services, including those unrelated to COVID-19, through Dec. 31, 2020; we also authorized a 90-day mail-order benefit for refills of all applicable prescriptions, allowing members to remain in their homes as much as possible.
As the region’s leading community based, not-for-profit health plan, we also focus on the overall health of the entire community. We dedicated a team to reach out to members to offer support during this time of uncertainty and we’ve assisted more than 25,000 members since March. And, we’ve generously shared in community and foundation efforts to support local food banks and unemployed workers."
Univera Healthcare:
"The health plan provides coverage in full for diagnostic/viral testing as well as antibody testing that is determined to be medically appropriate for the diagnosis and treatment of an individual by an attending provider as evidenced by an order from the attending provider."
The tests must be FDA approved or the subject of an emergency use order request and the lab performing the testing must be appropriately certified.
This policy on COVID-19 testing applies to members in all lines of business: commercial plans, Medicaid Managed Care plans and Medicare Advantage plans.
Testing that is ordered or performed solely for purposes of pandemic control or re-opening the economy, and not based on a determination by an attending provider that the test is medically appropriate for the diagnosis and treatment of an individual member, is not covered. This includes tests performed on an asymptomatic individual solely to assess health status as required by parties such as a government/public health agency, employer, school, or camp.
Independent Health:
“Independent Health continues to cover COVID-19 testing with no cost-sharing when a healthcare provider decides that testing is medically appropriate for the purpose of diagnosing or treating our members.
Based on federal guidance, health plans are not required to cover COVID-19 testing when it is to screen for “return to work/school” purposes or for public health surveillance. Our policy follows this federal guidance and is consistent with other health plans throughout New York State and across the country.”